Transmucosal permeability refers to the transport of material such as drugs across the oral mucosa. Transmucosal permeability is a unique approach that aims at delivering the drug systemically through the oral mucosa. (rather than delivering drugs that produce a local effect on the oral mucosa, as is the case in mucosal drug delivery.)

As an alternative to enteral delivery of drugs, this route of drug delivery is less invasive. It doesn’t require much technical equipment. The main consideration with transmucosal delivery is that the absorption via this route is variable. Thus, making it unsuitable for delivering low potent drugs.
Transmucosal permeability: methods for drug absorption
Drugs traverse through the oral mucosa by different methods of absorption. Some of the commonly adopted routes are :
- Passive diffusion refers to the non – ionic diffusion of drugs from the high concentration to the lower concentration and is the major absorption process.
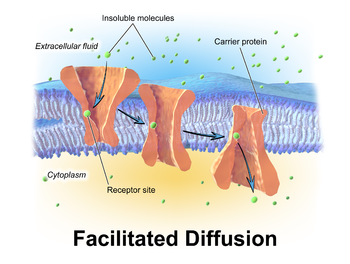
- Facilitated diffusion – This is similar to passive diffusion but differs because it uses integral transmembrane proteins to facilitate the transport.

- Active transport – This transport requires energy for the drug’s movement across the oral mucosa. The hydrolysis of ATP often provides the energy.
- Pinocytosis – In this type of transport, the entire drug molecule is engulfed into the cell as a small vesicle. This process also requires energy in the form of ATP.
The following factors must be considered, To ensure that the transmucosal route can successfully deliver a drug. Factors affecting Transmucosal permeability are:
- Lipophilicity of the drug – The permeability is higher for agents or drugs that are highly lipid-soluble.
- Salivary secretion – Higher the salivary secretion, the higher the drug’s chances of being flushed out. This can lead to incomplete absorption of the drug.
- The saliva’s pH – Absorption is favored when the pH is around 6.
- Binding to the oral mucosa – Proper binding of the drug carrier to the oral mucosa is essential. It helps permeates the drug across the mucosa to the systemic circulation.
- Oral epithelium thickness – The permeation rate of the drug from the drug carrier is dependent on the thickness of the oral epithelium. The thicker this layer, the longer the residence time of the drug.
Formulation considerations of the Buccal Delivery Systems :

Buccal delivery systems refer to the administration of the drugs via the buccal mucosa. The buccal mucosa is the mucosa that lines the inner cheek. Formulations targeting this region are placed in the mouth between the upper gums and the cheek. This mucosa is highly vascularized and is relatively easy to access. The absorption of drugs in this region mainly occurs by passive diffusion into the lipoidal membrane. The various buccal formulations currently available in the market are buccal tablets, buccal patches/films, and buccal gels/ointments.
The main factors that must be considered before formulating these buccal delivery systems are :
- Size of the formulation – Formulations with a size of 1 to 3 cm2 and a daily dose of 25 mg or less is preferred.
- The drug’s molecular weight – Drugs with high molecular weight cannot readily permeate through the buccal mucosa. Hence low molecular weight drugs are often preferred. To facilitate the delivery of the former, penetration enhancers are used.
- Nature of the drug – Highly lipophilic drugs that can passively diffuse through the buccal mucosa is used while formulating buccal drug delivery systems.
- The pH of the formulation – The pH of the carrier used in the system alters the drug’s absorption. Lowering the carrier pH increases some drugs’ absorption, while the opposite is true for other drugs.
- Physicochemical characteristics of the drug – The drug should be odorless and not have an unpleasant taste.
Due to the saliva’s washing effect and the mechanical stress, the drugs in these formulations are quickly removed from the oral cavity. Thus, to ensure an optimum therapeutic effect, the formulation must contain an optimum mucoadhesive agent. This helps maintain an intimate and prolonged contact of the formulation with the absorption site for at least 4 to 6 hours.
Excipients used for the formulation of buccal drug delivery
The commonly used excipients for the formulation of buccal drug delivery systems are :

- Mucoadhesive polymers – These synthetic or natural polymers interact with the mucosa’s epithelial surface to adhere to the mucosal layer. The commonly used polymers in buccal dry or partially hydrated dosage forms are polyacrylic acid, polyvinyl alcohol, sodium carboxymethyl cellulose, and sodium alginate.
- Penetration enhancers – These substances increase the buccal mucosal membrane permeation rate. It also aids the delivery of drugs that have high molecular weight and are easily inactivated. E.g., Sodium laurate, sodium taurocholate, oleic acid, and chitosan, among others.
- Enzyme inhibitors – are added to prevent the degradation of the drugs, especially peptides, or by the mucosal enzymes. These inhibitors also improve the drugs’ buccal absorption: Eg. Aprotinin, bestatin, puromycin, and bile salts.

Pingback: General concepts in mucosal drug delivery > PharmaCampus
Best notes for Pharma student
Thanku Pharmacampus